The blind spot of anaesthesiology
Niek Sperna Weiland on his pioneering work to reduce the use of anaesthetic gases.
4 November 2024
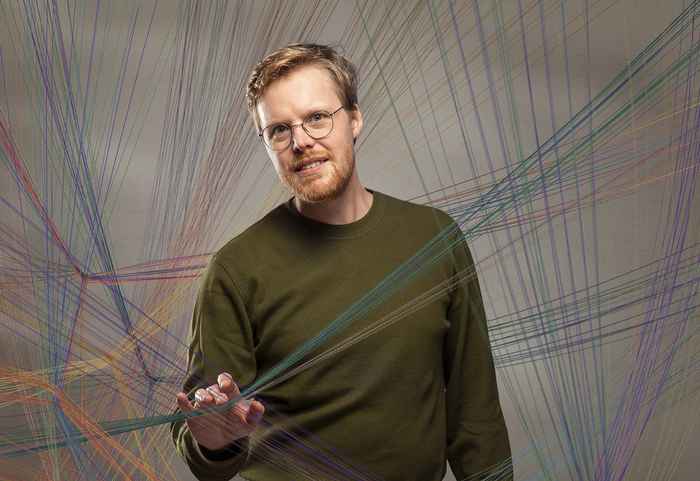
Niek still has his surgical cap on when he comes running in for the interview. He might get paged at any moment to return to his patient. It’s not just any cap, it’s the Selma, named after his colleague who worked hardest to develop this washable hat and get it included in the supplier's catalogue. ‘A no-brainer,’ he smiles. ‘We’re now converting the entire hospital to washable caps, so w’re suddenly going from 100,000 disposable caps to 500 reusable ones a year.’
His plans for SEVEN are also starting to take shape. Niek: ‘I hope that in five years, we’ll have completed a major project in which a vision has been developed of what healthcare should look like in 2050, as well as a roadmap of how to get there. I hope that some test cases will have been done by then that prove that the plan is feasible and that we have a model that can be copied to other healthcare sectors.’
When asked whether he can remember when and where his commitment to environment and climate started. Niek answers promptly: New York, 2016. During an exchange programme at New York University, he heard anaesthesiologist Kate Huncke speak about sustainability there, and he suddenly realised that it was an obvious fit to combine his two major interests: anaesthesiology and care for the planet. Barely two years later, he was already setting up a Green Team for the operating room (OR) at Amsterdam UMC. At the time, he thought it was the first in the Netherlands, but later he discovered that Leiden UMC had set one up more or less simultaneously.
Stunned colleagues
Niek started with a small multidisciplinary team and began to delve into the existing literature. The footprint of an operating theatre consists of three components: anaesthetic gases, energy consumption and material use. Since anaesthetic gases fall directly within the responsibility of his profession and he could convince his own department fairly easily, he decided to start there. The amount of anaesthetic gas that enters the atmosphere is, of course, much smaller than that of carbon dioxide, but anaesthetic gases retain heat much better than CO2. Some of these are almost 7,000 times stronger greenhouse gases than CO2.
His first lecture on the climate effects of these gases made his colleagues do a double take. They were stunned that they had never heard about this before and were soon ready to switch to alternative drugs that can be administered by infusion. The Amsterdam UMC decided to immediately stop using the two most harmful types of anaesthetic gas and reduced the use of the other gases by 75% over six years. Together, the eight Dutch UMCs are already saving 3.5 kilotonnes of CO2 emissions per year. Niek: ‘That reduced the footprint of the teaching hospitals enormously. But of course I was already looking outwards and wondering how I could bring others into this.’
Urgenda's Measure 51
Niek decided to contact Urgenda, because he finds their approach so sympathetic. Niek: ‘They really go the extra mile and show the government what can be done to meet the climate targets.’ At the time, the environmental organisation was working on a list of 54 measures that would enable the government to meet its 25% CO2 reduction target by 2020. Niek was asked to provide the figures, and ‘other ways to give anaesthesia ’ ended up as measure 51 in the Action Plan.
Of the total emissions from the Dutch healthcare sector – 11 megatonnes of CO2 equivalents, whoch is about 7% of total national emissions – a reduction of 0.1 megatonnes CO2 equivalents could be achieved with anaesthetic gases. With hindsight, he admits, this was slightly overestimated. But since no national figures existed, he had to rely on those from abroad. The estimate led to a government subsidy of one million euros, half of which was to be spent on reducing energy consumption in the OR and the other half specifically on reducing anaesthetic gases.
Environmentally friendly methods of anaesthesia lead to less nausea, less confusion, better recovery and did not increase the risk of complications
Win-win situation
Thorough research was then of course needed into what the effects might be for patients. Niek: ‘The surprising outcome of this meta-analysis, a compilation of previous comparative studies among more than 70,000 patients in several countries, was that the environmentally friendly methods of anaesthesia lead to less nausea, less confusion, better recovery and did not increase the risk of complications.’ The analysis led to publications in what Niek considers to be the world's top anaesthesia journal, the British Journal of Anaesthesia, and in the The Lancet eClinicalMedicine.
This compelling evidence led to much international interest and a trip to China with a trade delegation from the Dutch Ministry of Health, Welfare and Sports to open Chinese anaesthesiologists' eyes to the climate impact of anaesthetic gases. Niek: ‘I want to start with education and creating awareness in this area, to get to some kind of critical mass of people who want to do something about this, before moving onto measurements and a concrete plan.’
Niek is impressed by the active Green Teams in the Beijing Tiantan Hospital and Beijing Union Medical College Hospital he visited. And because the Chinese haven’t completely converted to diposable hospital materials from reusable ones, they don’t have to revert to reusable, with all the hygiene discussions that come with that. There's no need for him to convince the Chinese about the usefulness and necessity of the Selma.
Elles Tukker